SBAR (Situation, Background, Assessment, Recommendation) is a standardized method for relaying patient information in a fixed order. Clinicians use it during shift handoffs, rapid-response calls, phone consults, bedside updates, and unit-to-unit transfers across hospitals, clinics, long-term care, and telehealth. It keeps messages brief, specific, and oriented to the next step. Below is a collection of SBAR templates in Word, Google Docs, and PDF, ready to edit or print.
SBAR Templates
Psychiatric SBAR Template
Product Management SBAR Template
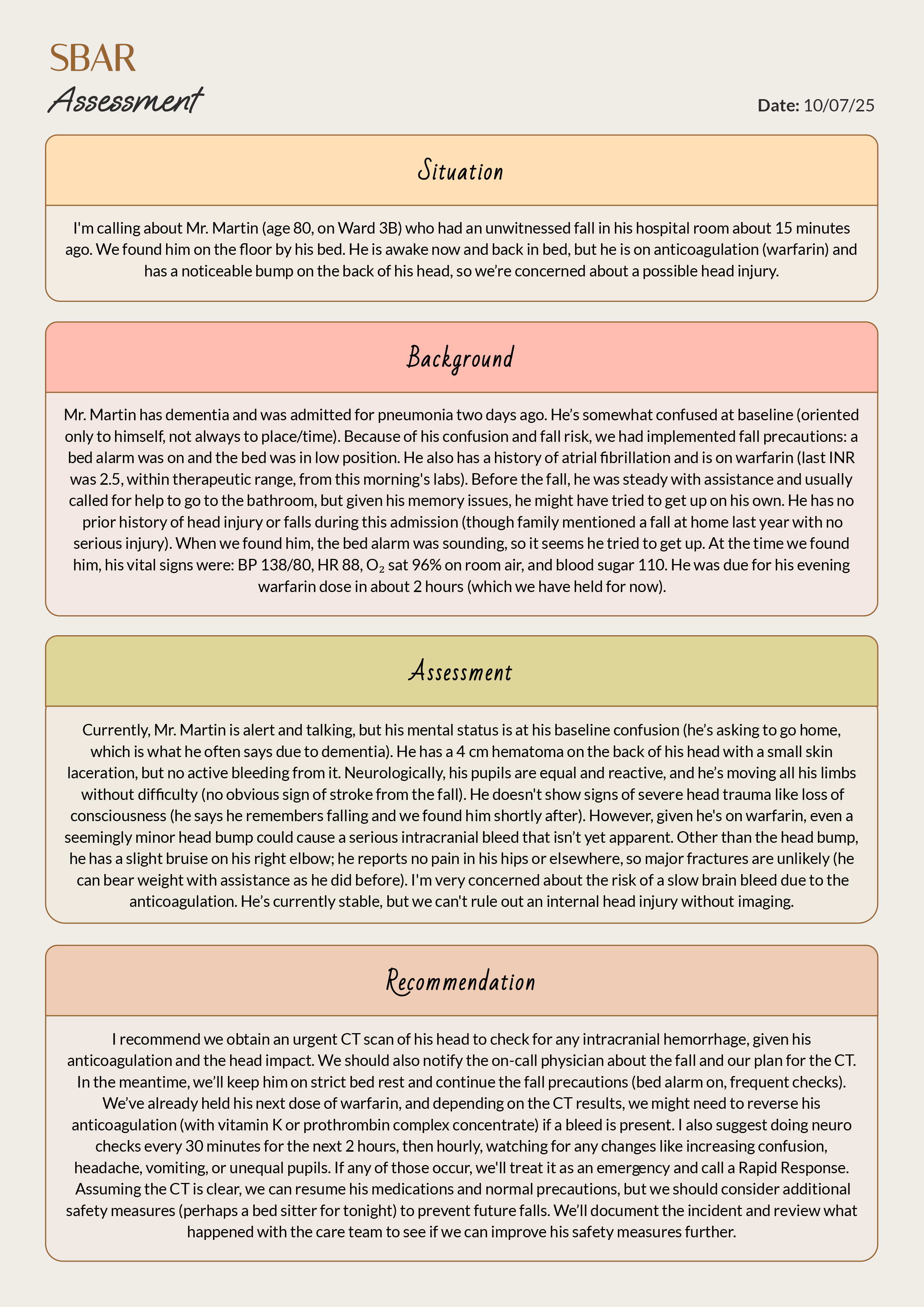
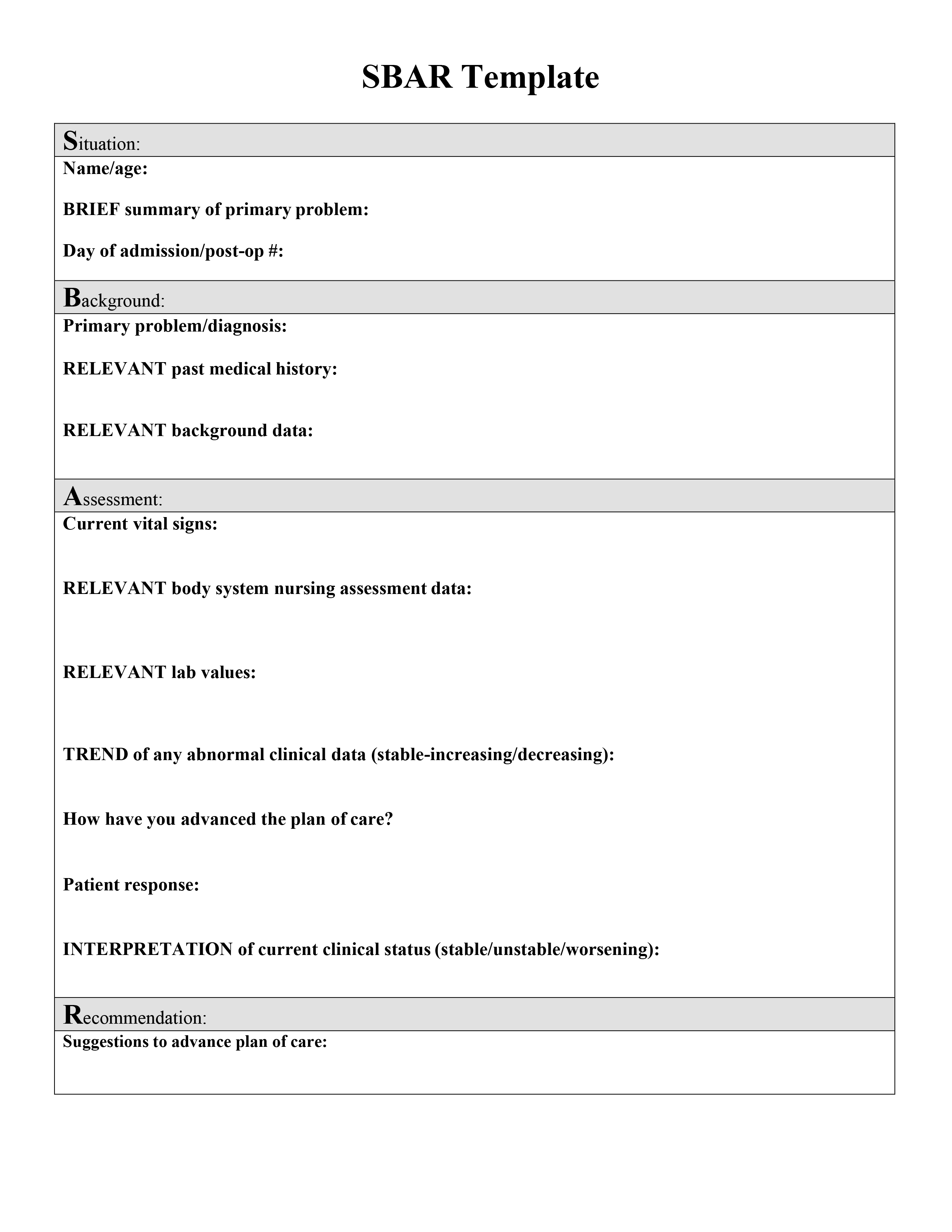
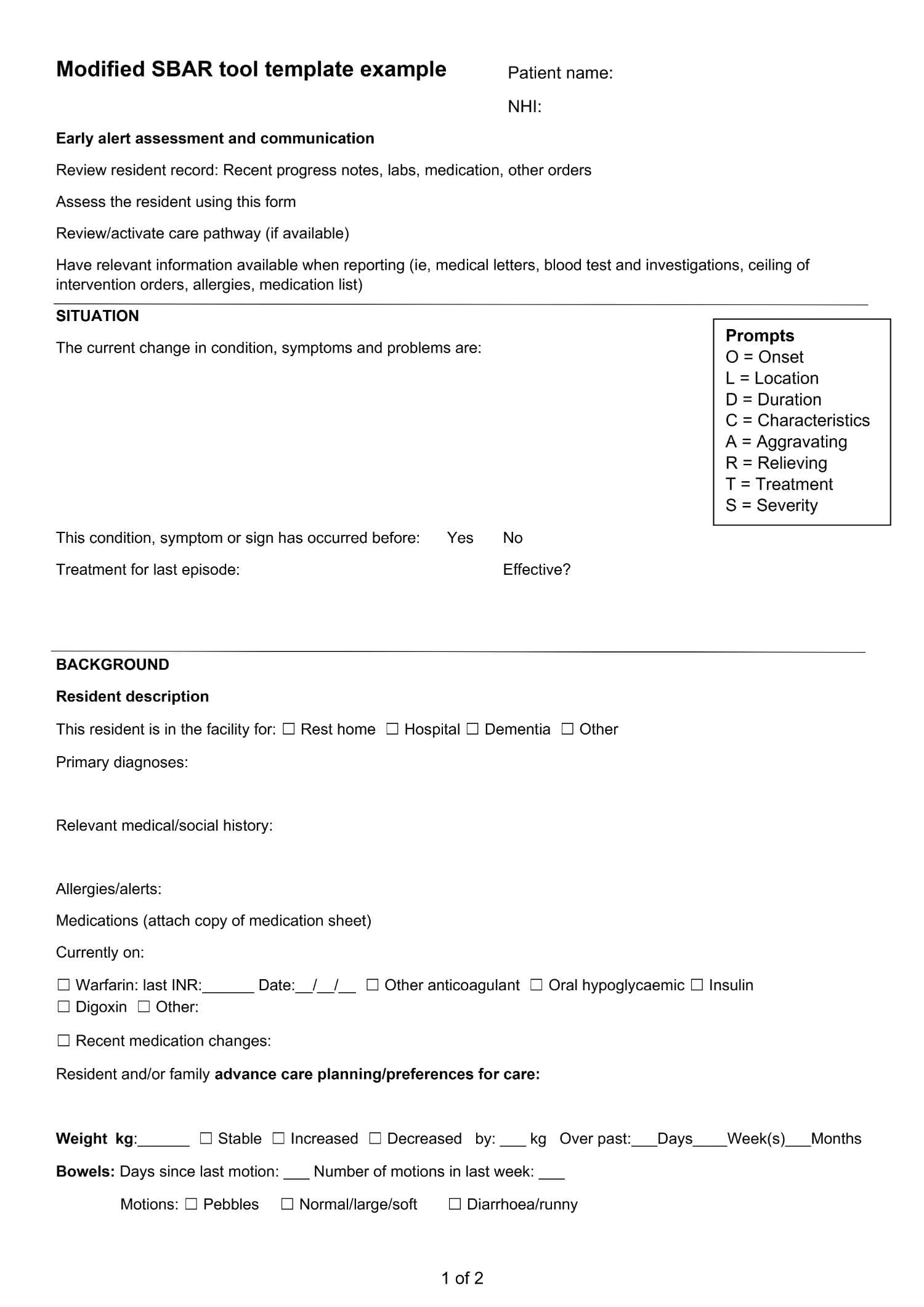
SBAR Assessment Template
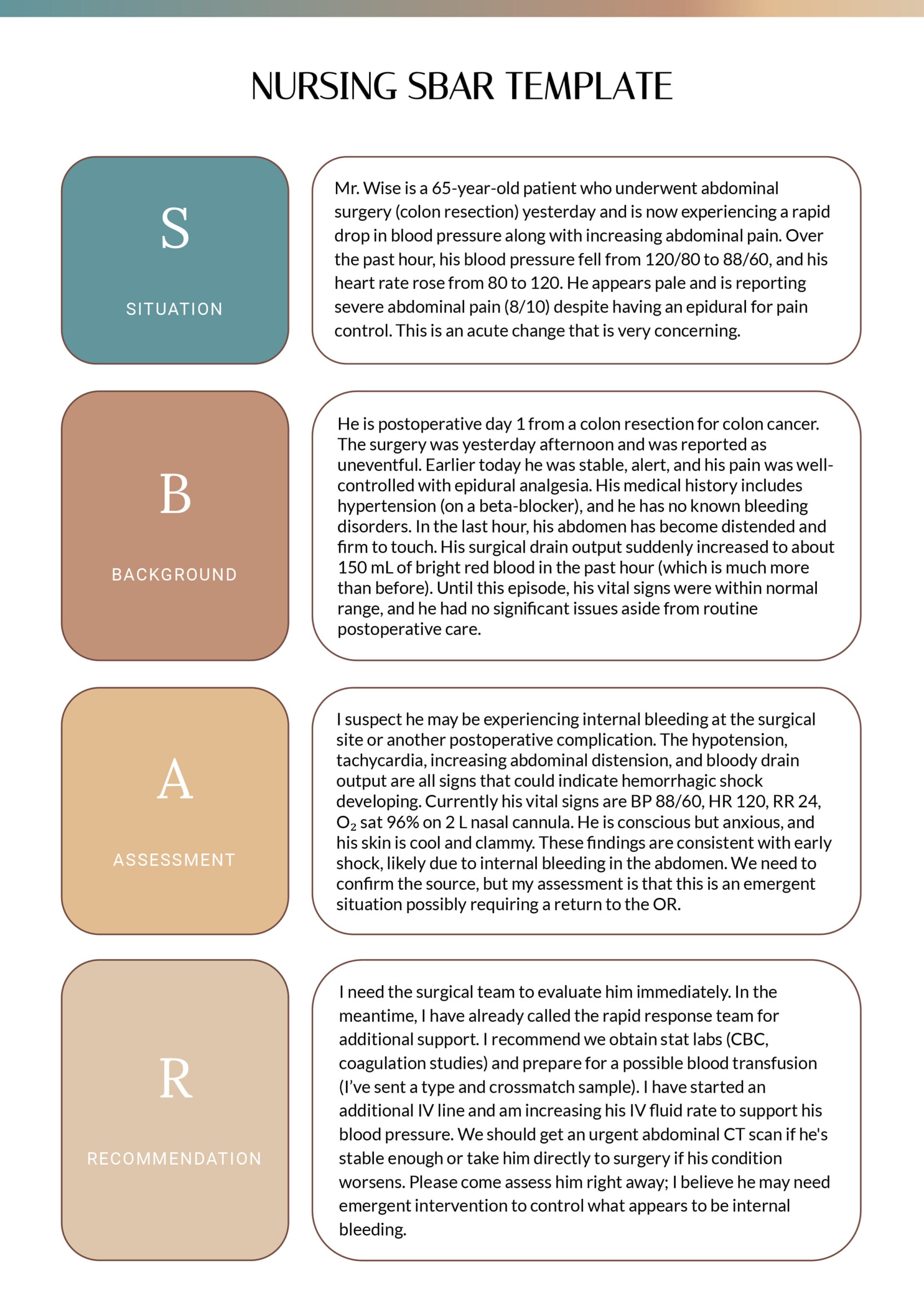
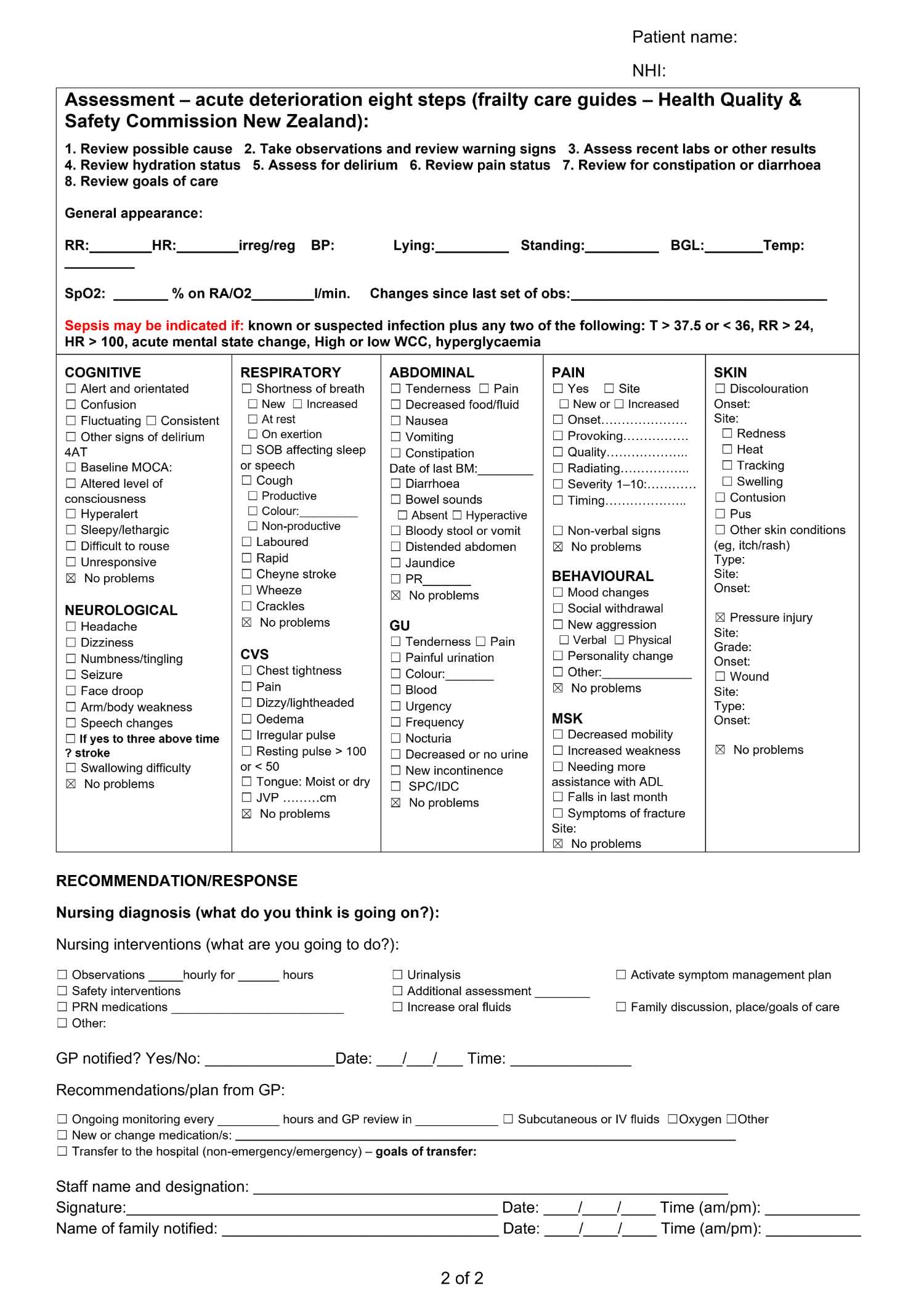
Nursing SBAR Template
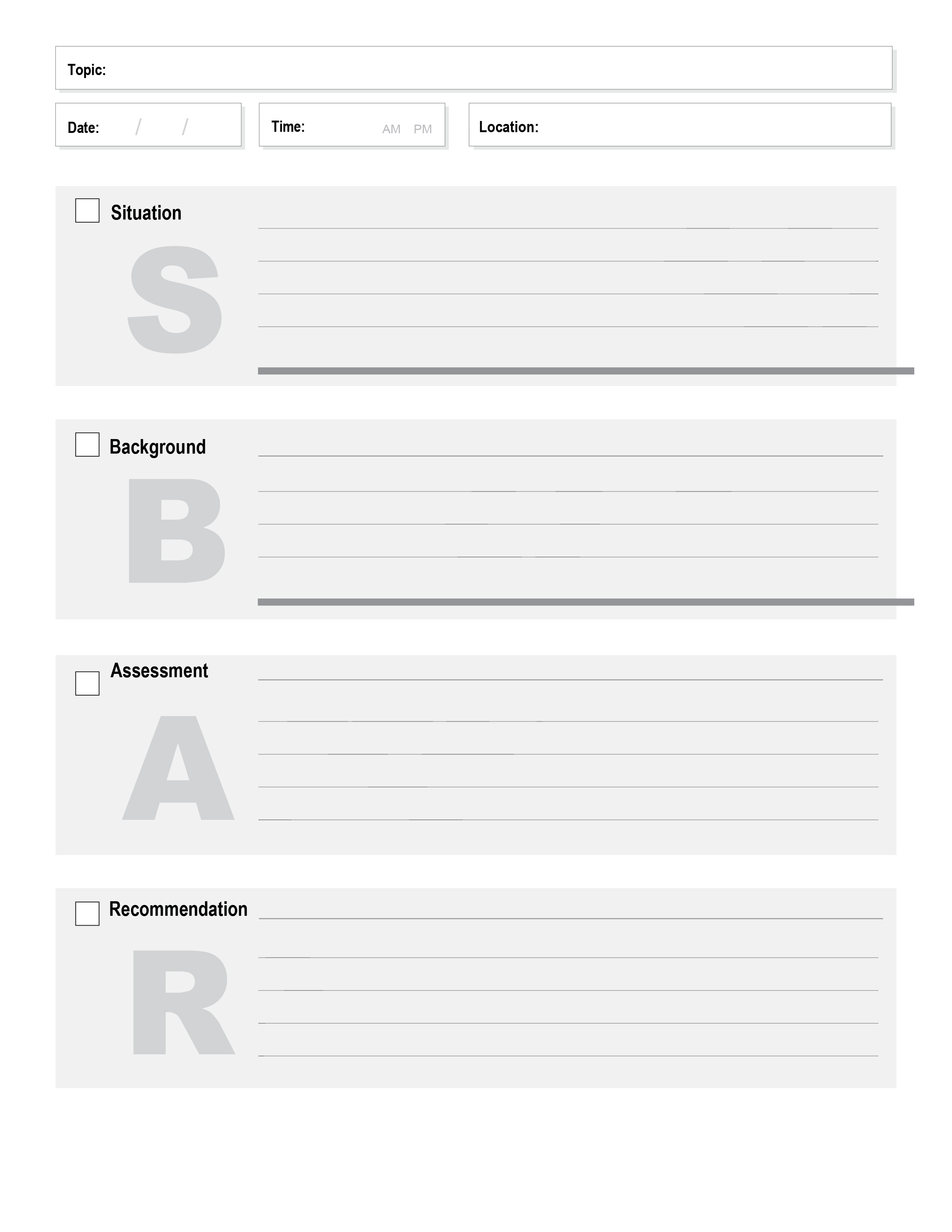
Handoff SBAR Template
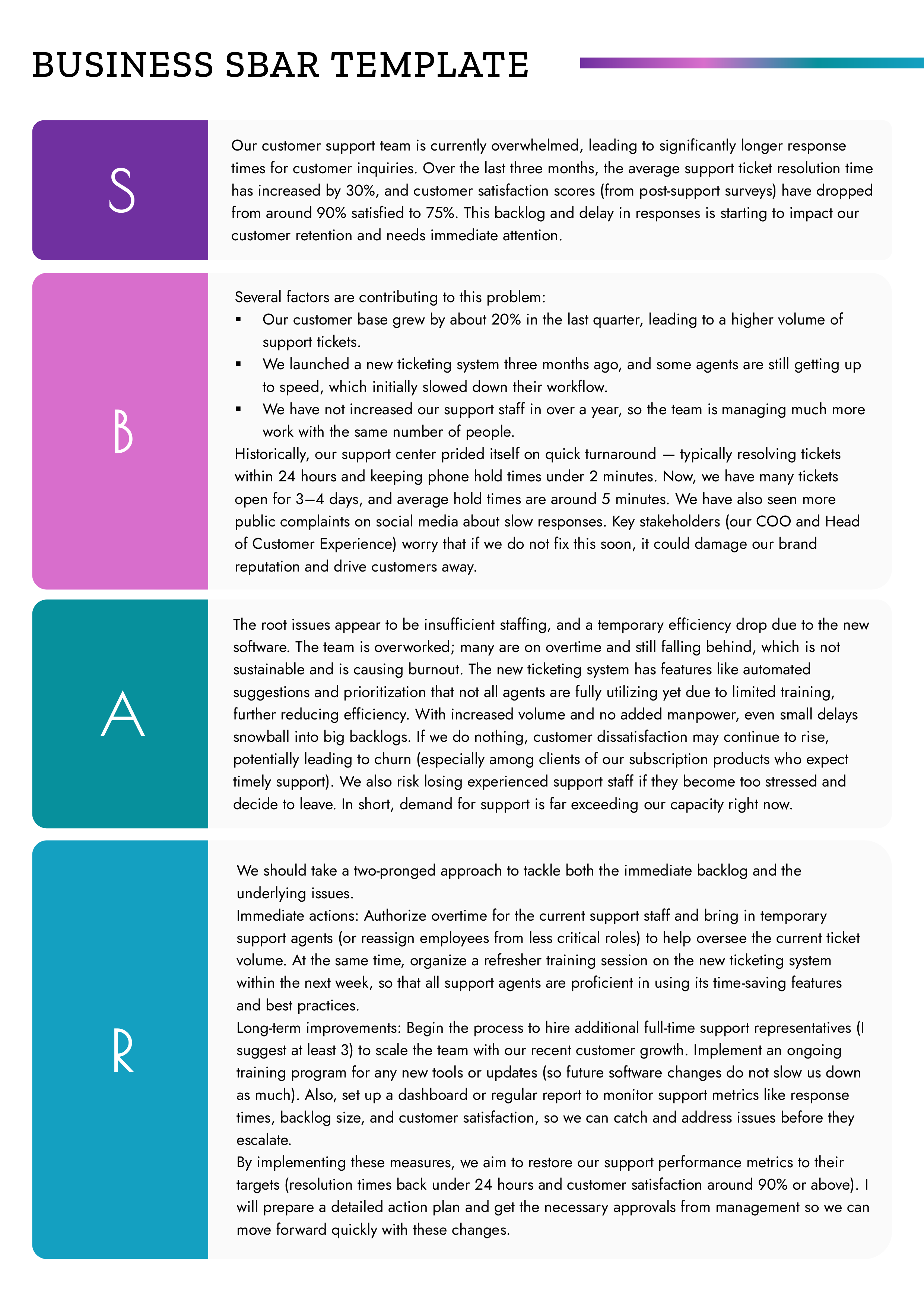
Business SBAR Template
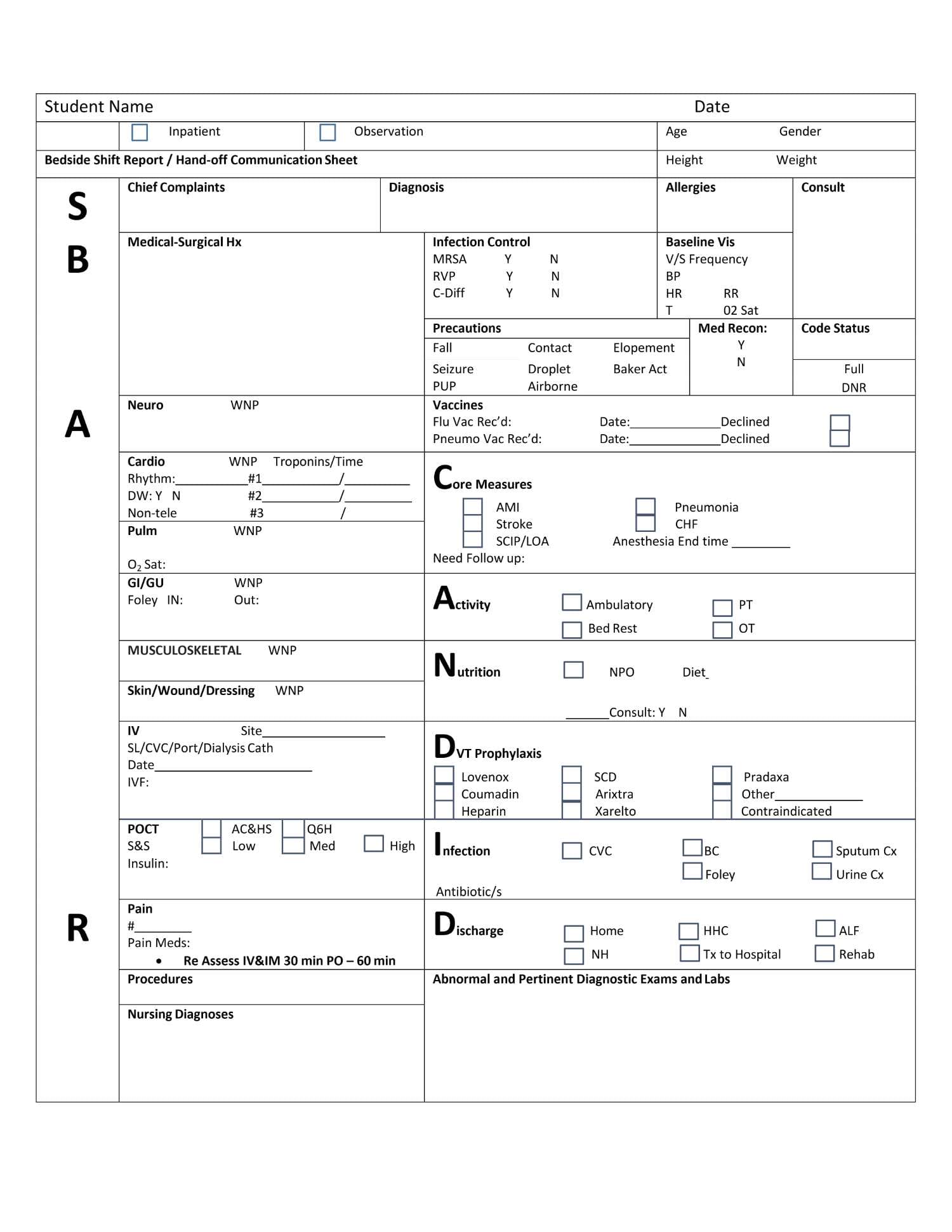
SBAR Shift Report Template
Critical Care SBAR
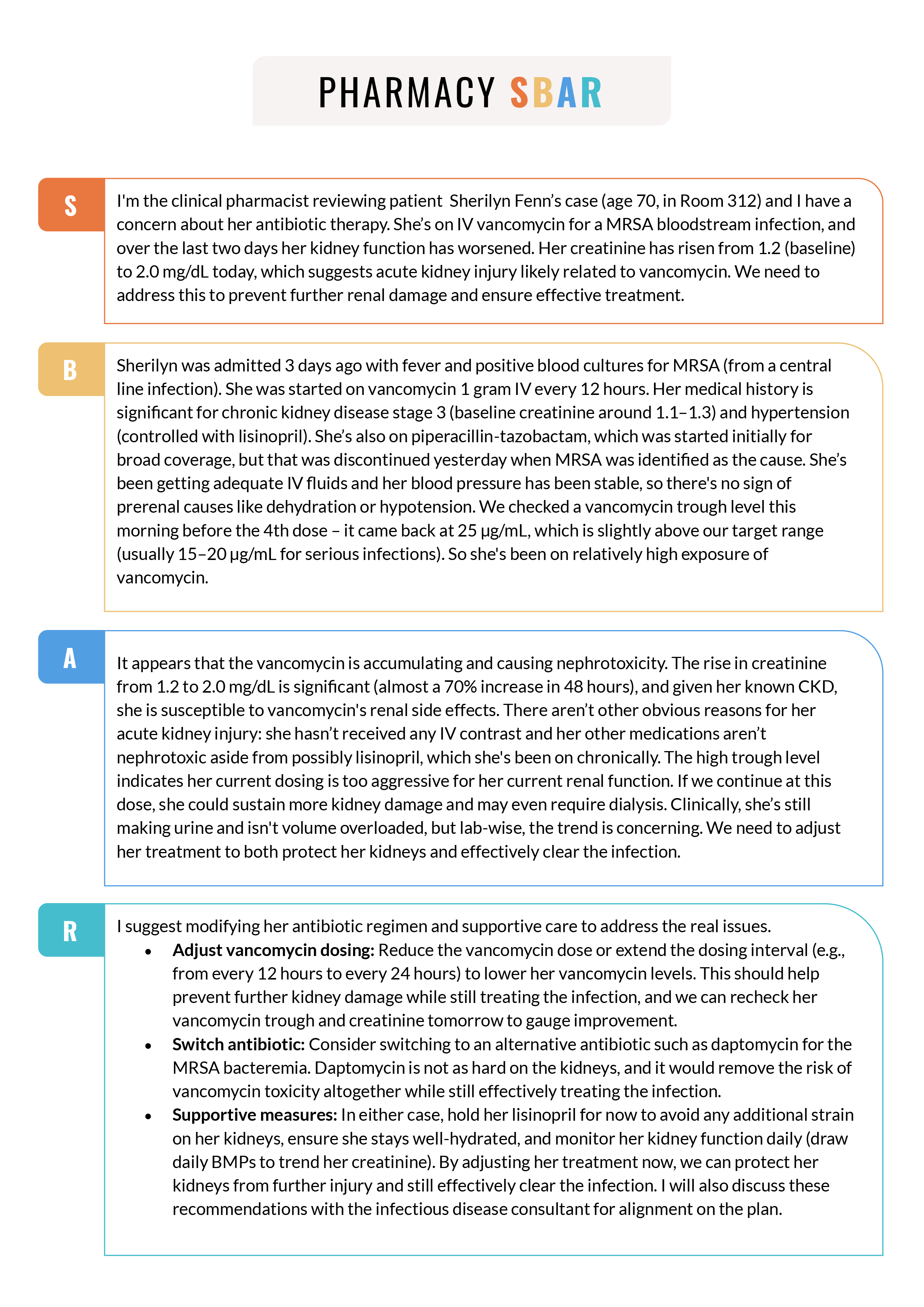
Pharmacy SBAR Template
Mental Health SBAR Template
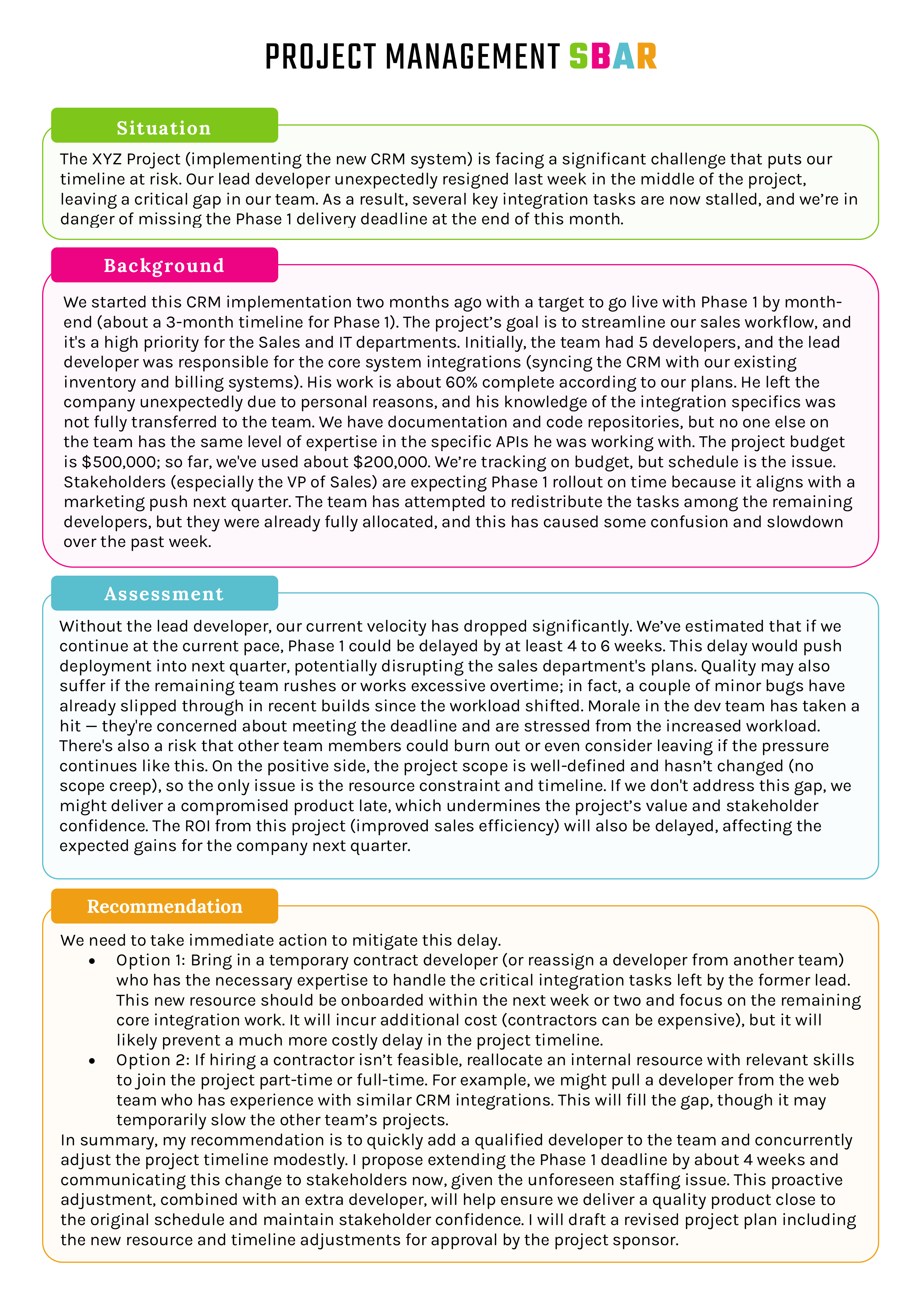
Project Management SBAR Template
Pediatric SBAR Template
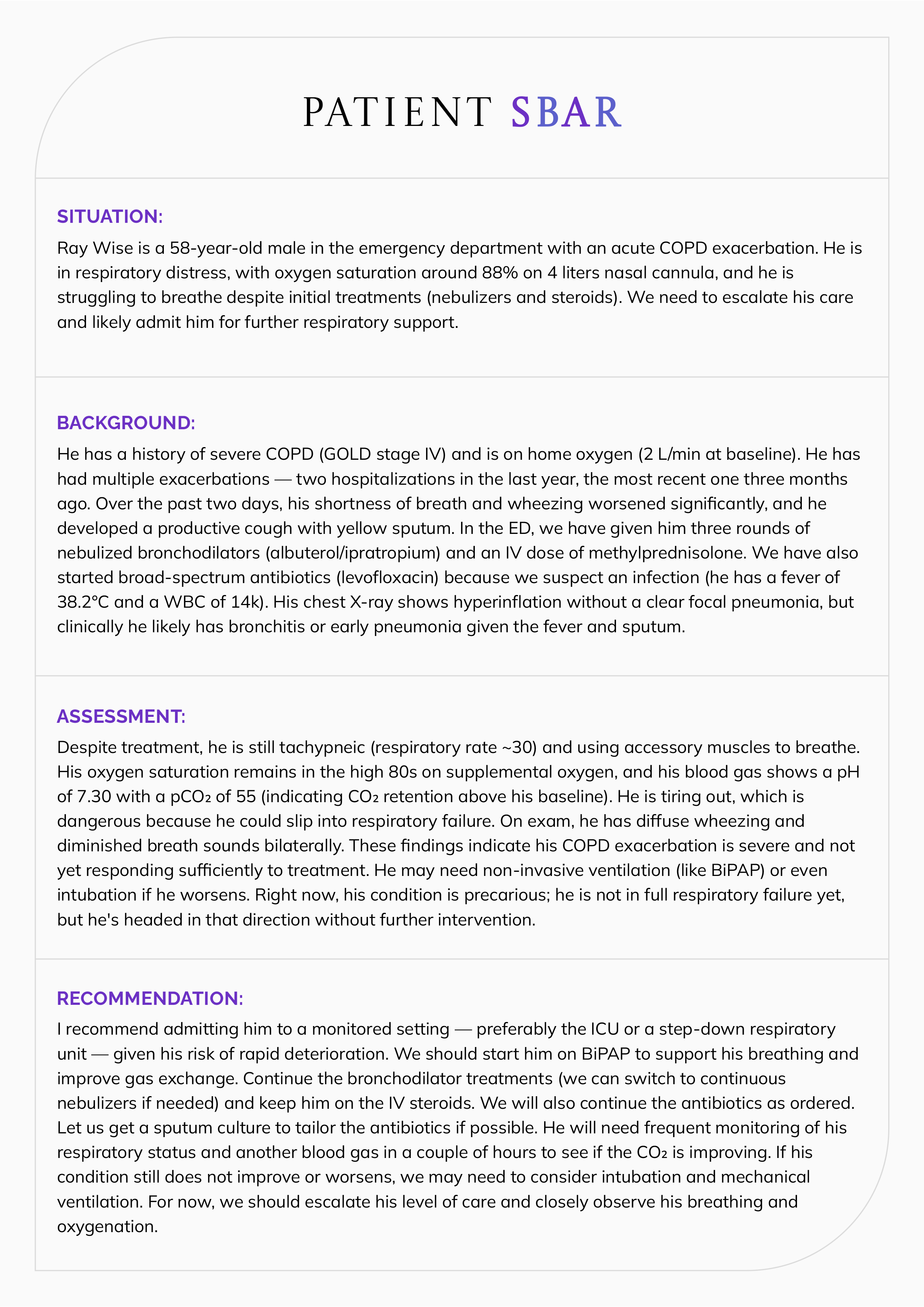
Patient SBAR Template
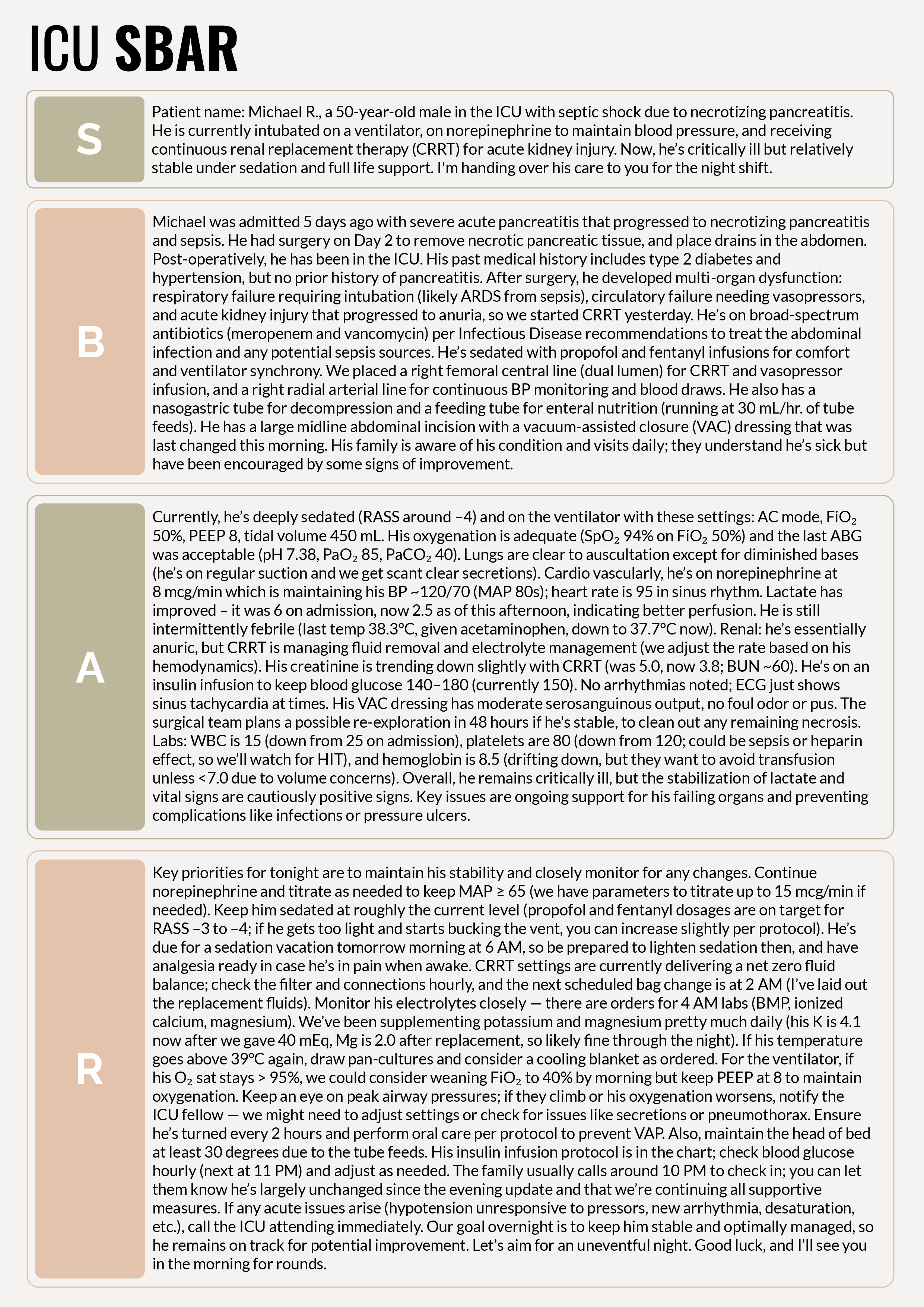
ICU SBAR Template
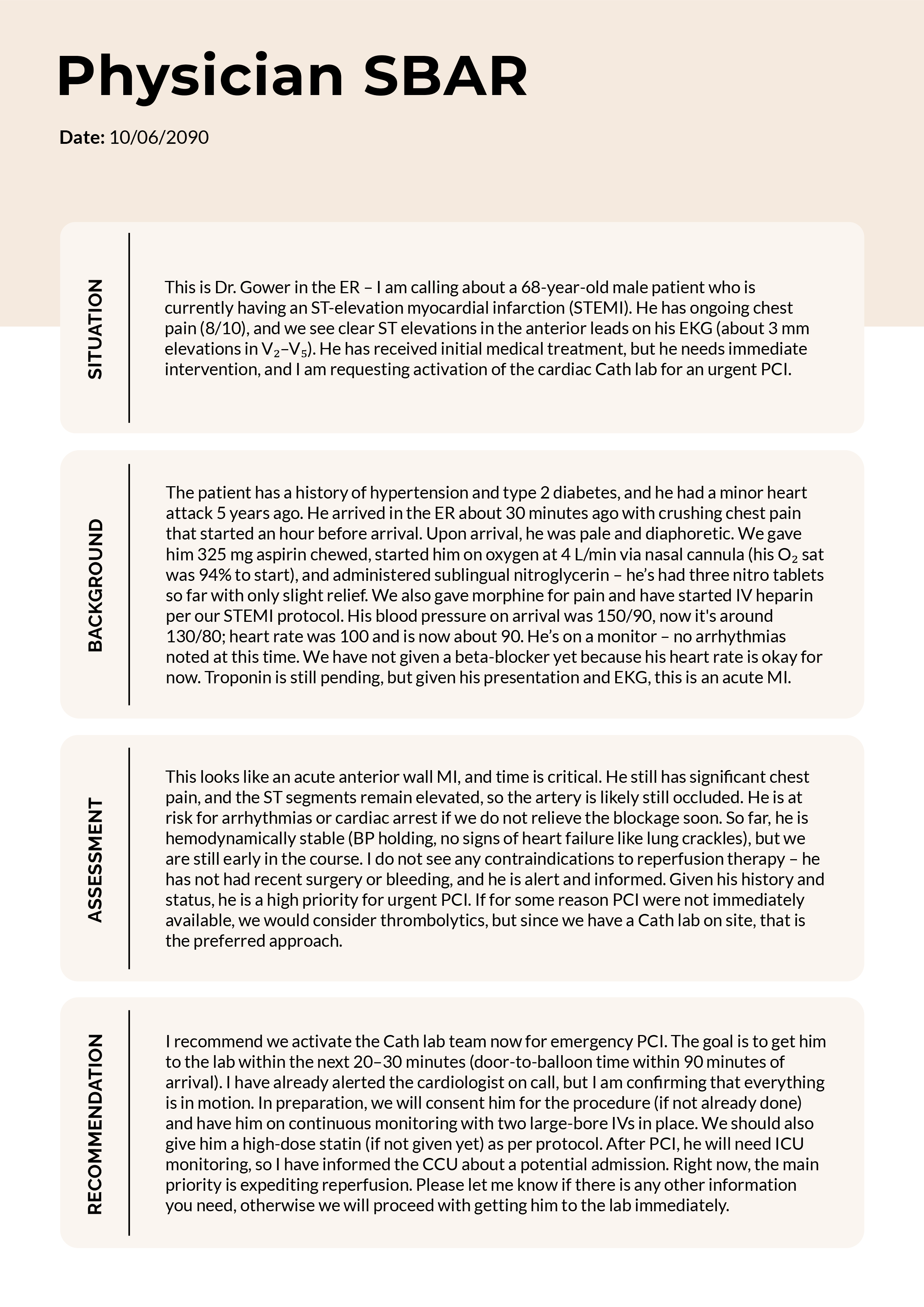
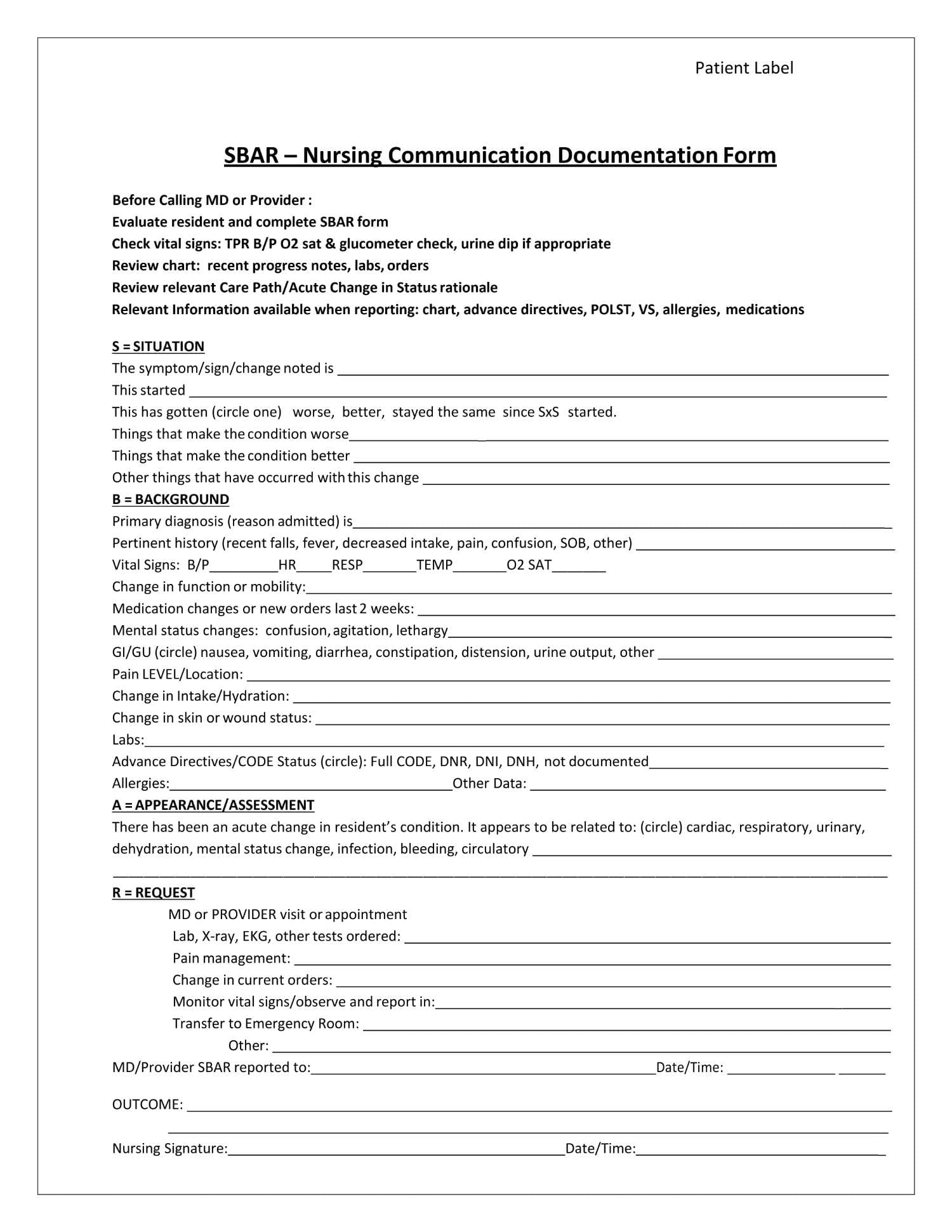
Physician SBAR Template
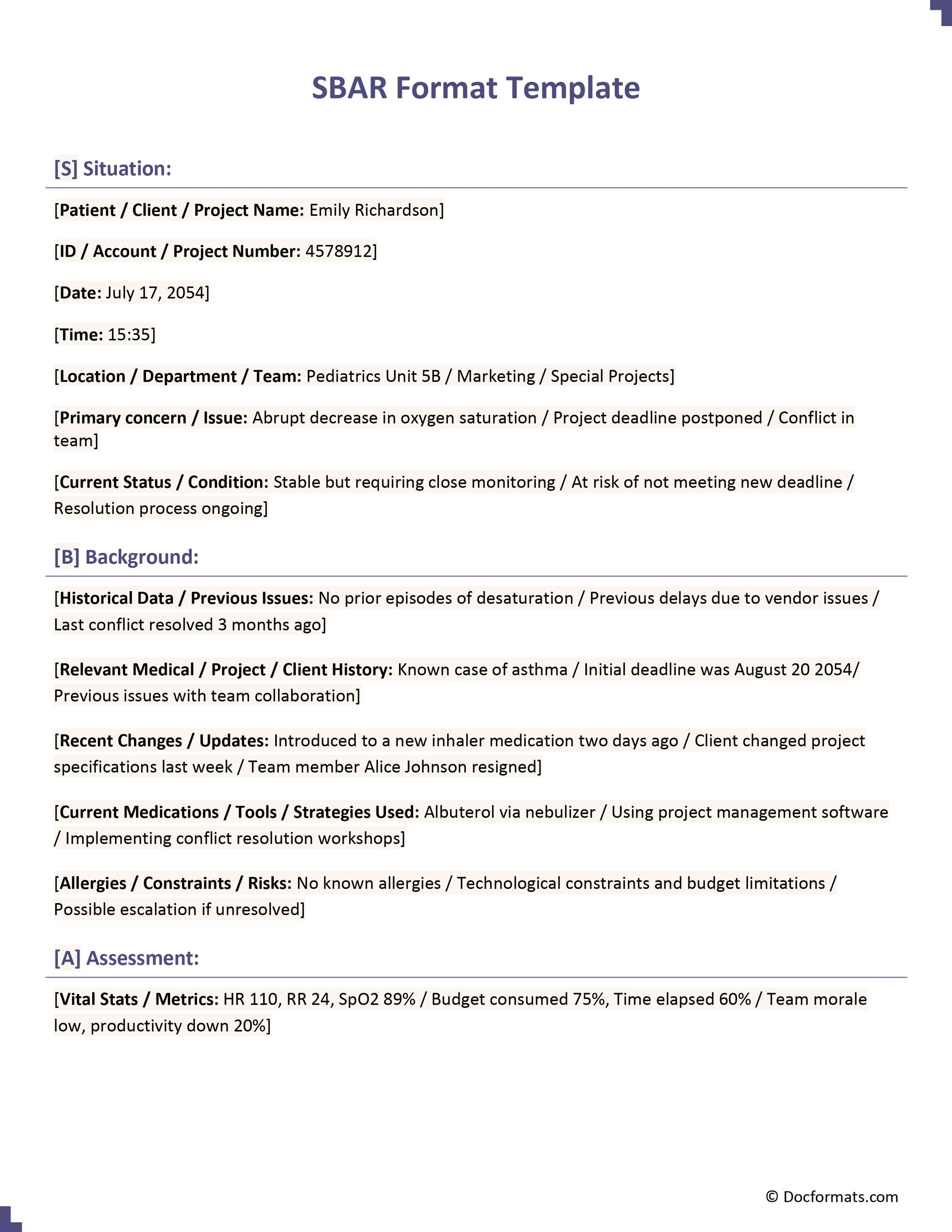
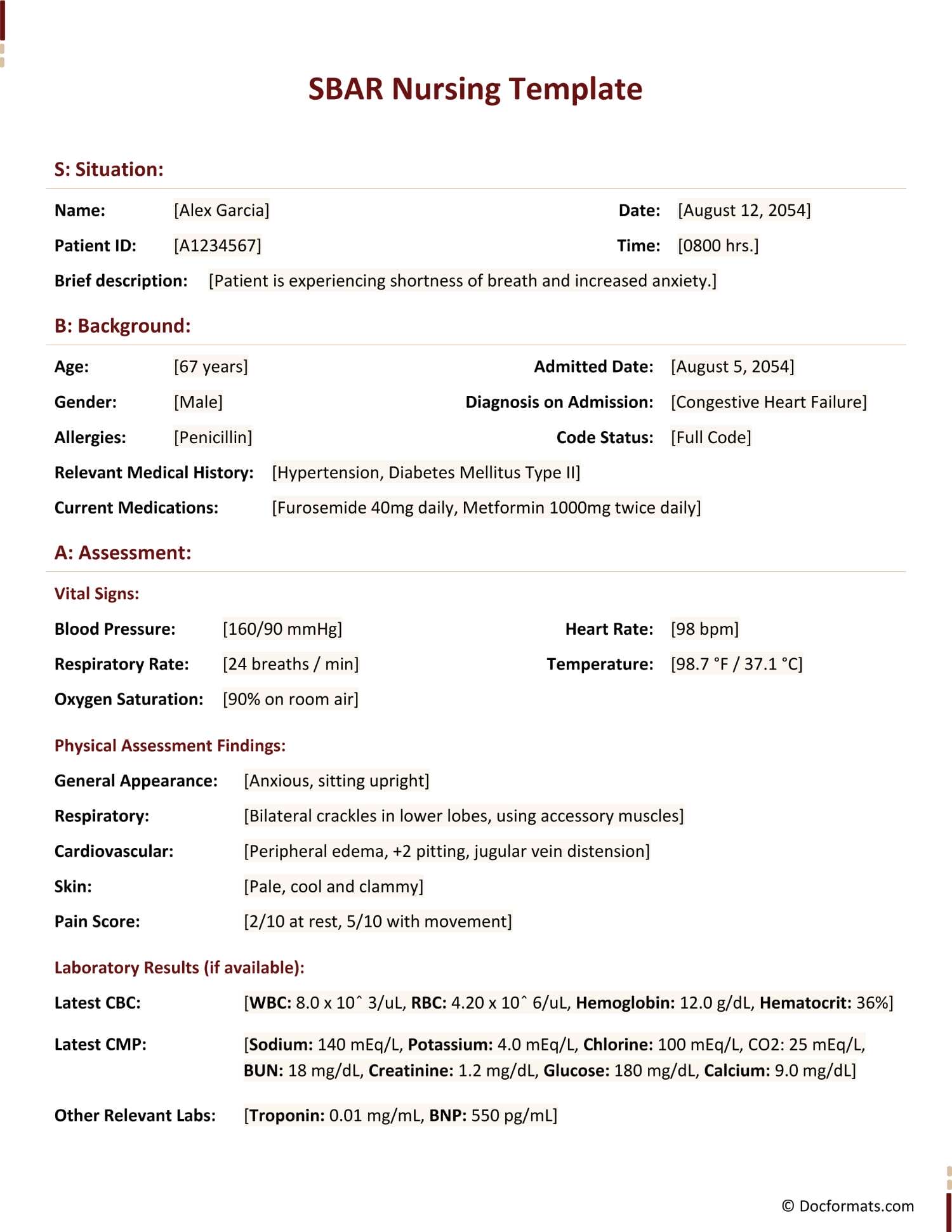
SBAR Format Template
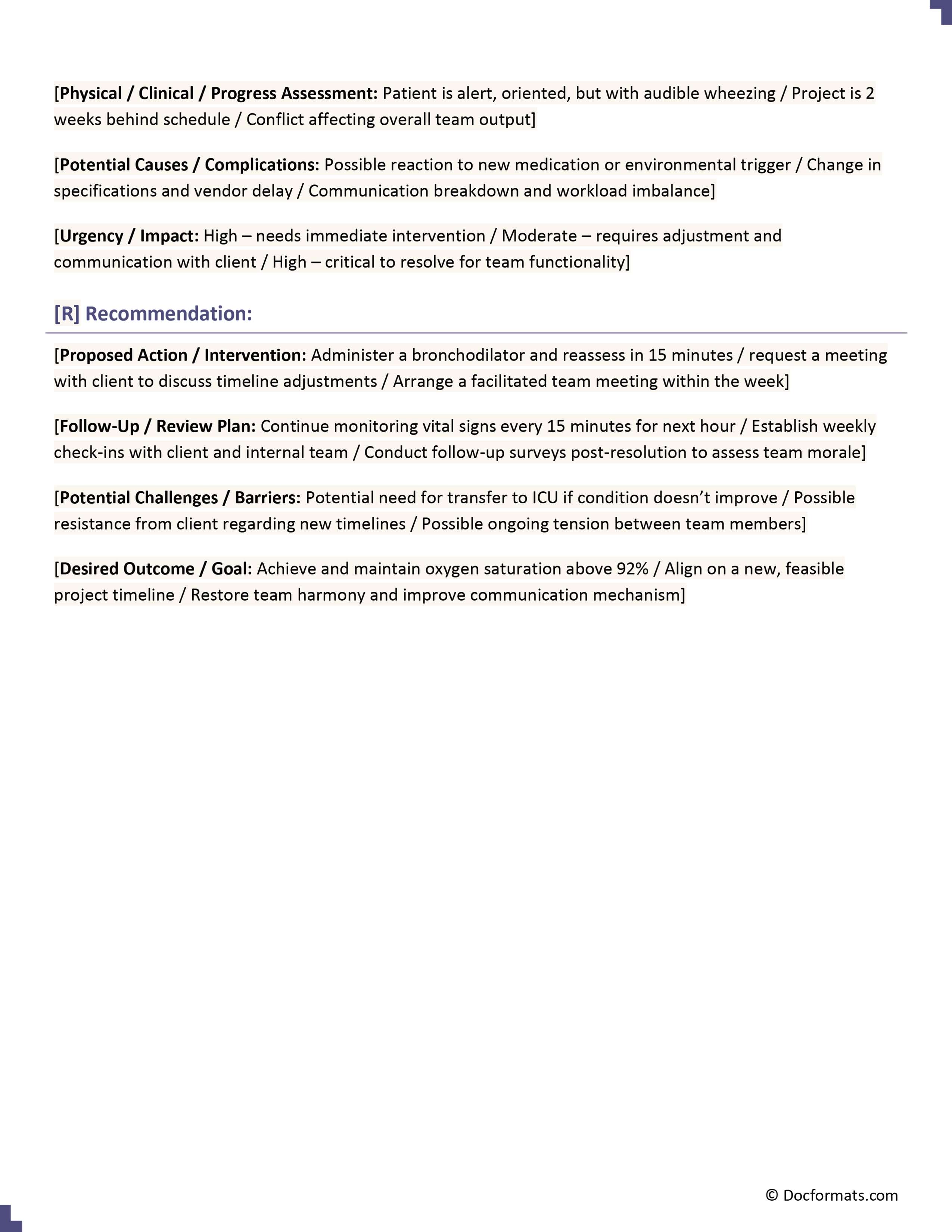
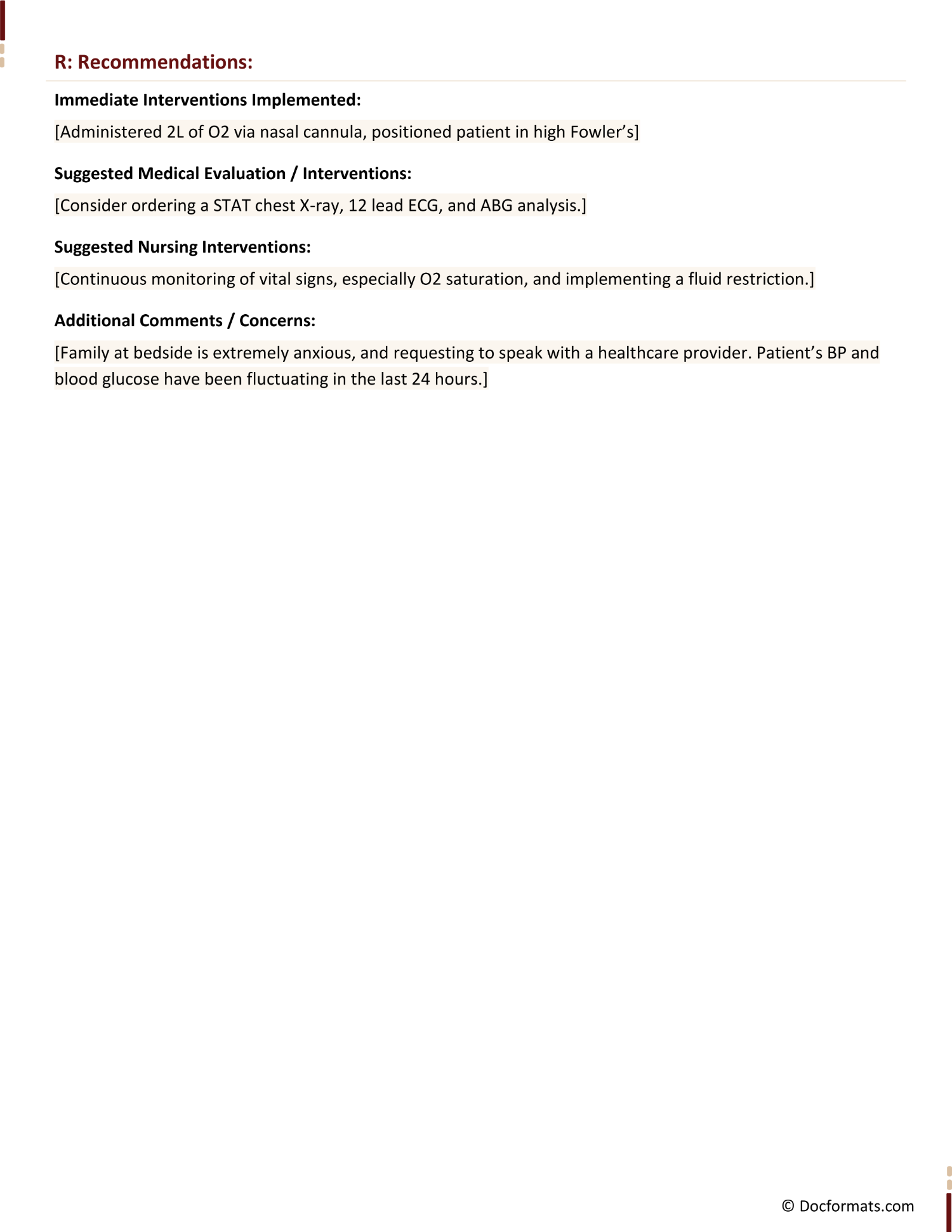
SBAR Nursing Template
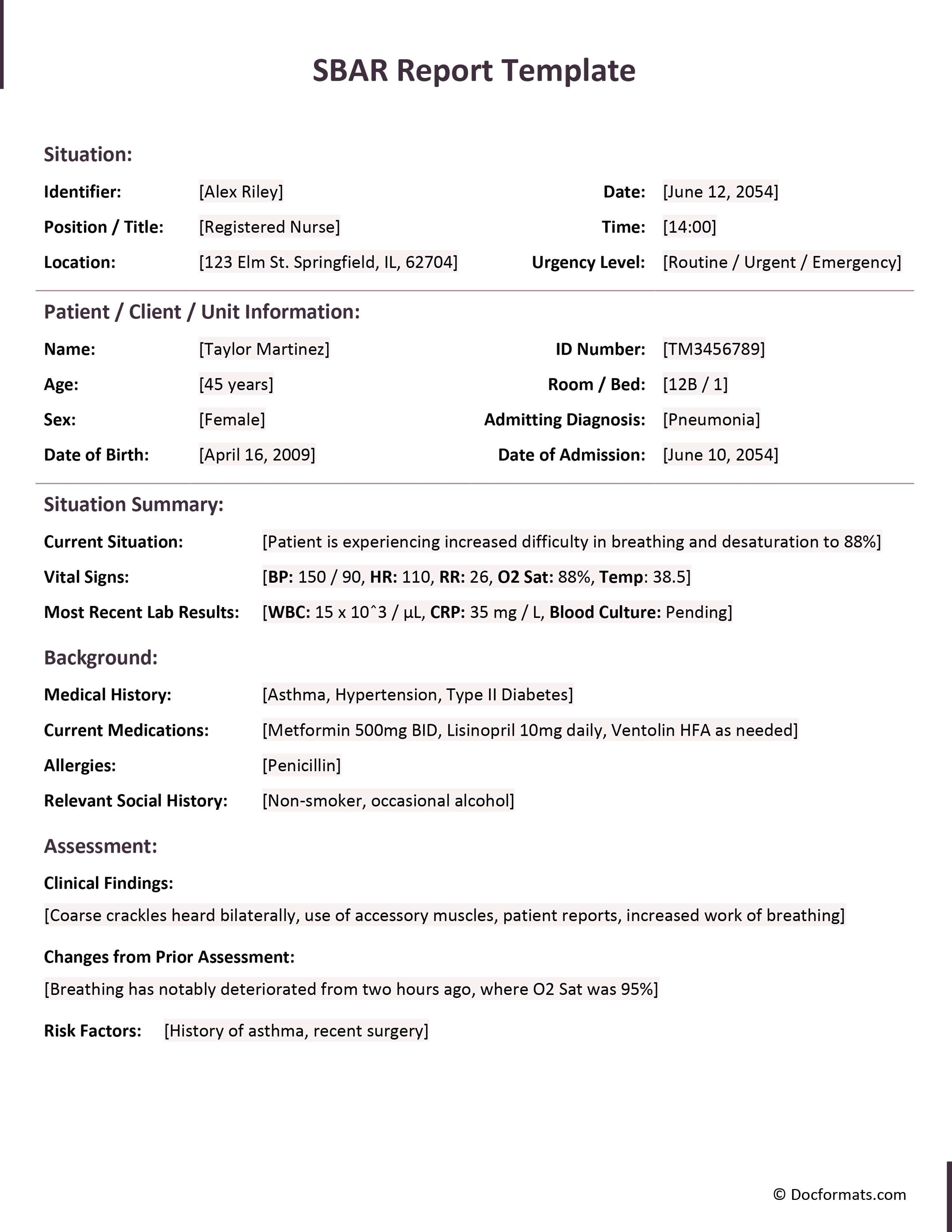
SBAR Report Template
SBAR Template
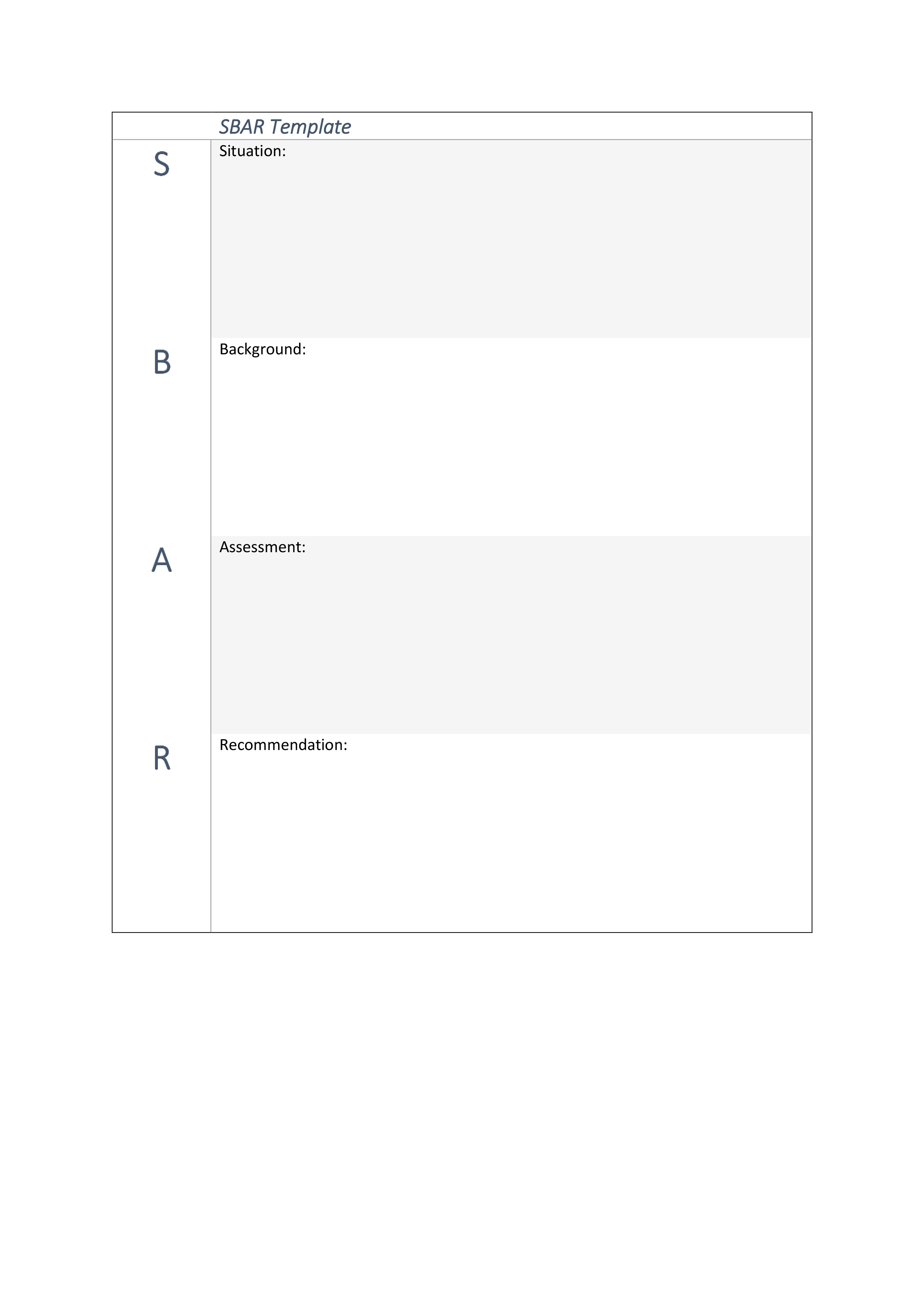
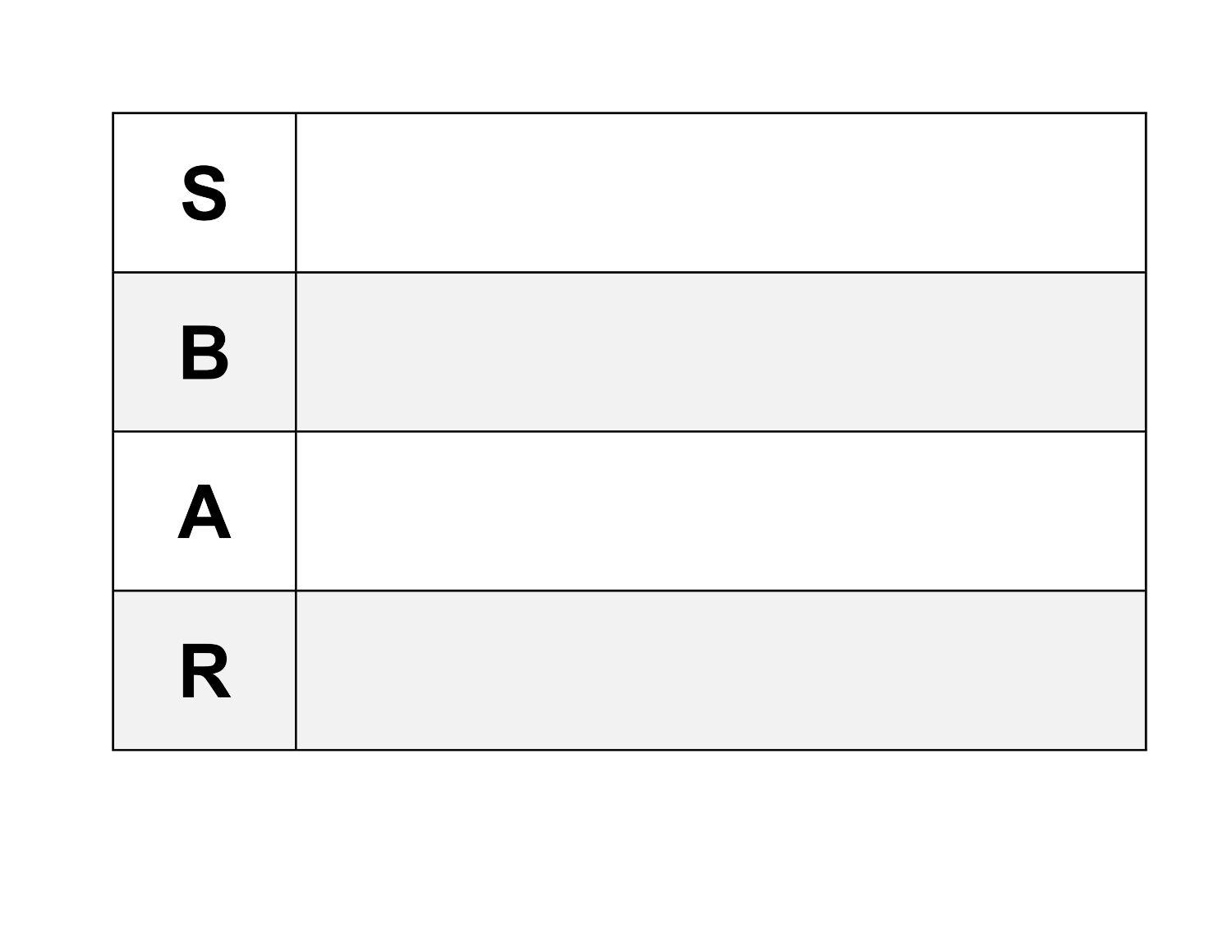
Blank SBAR Template
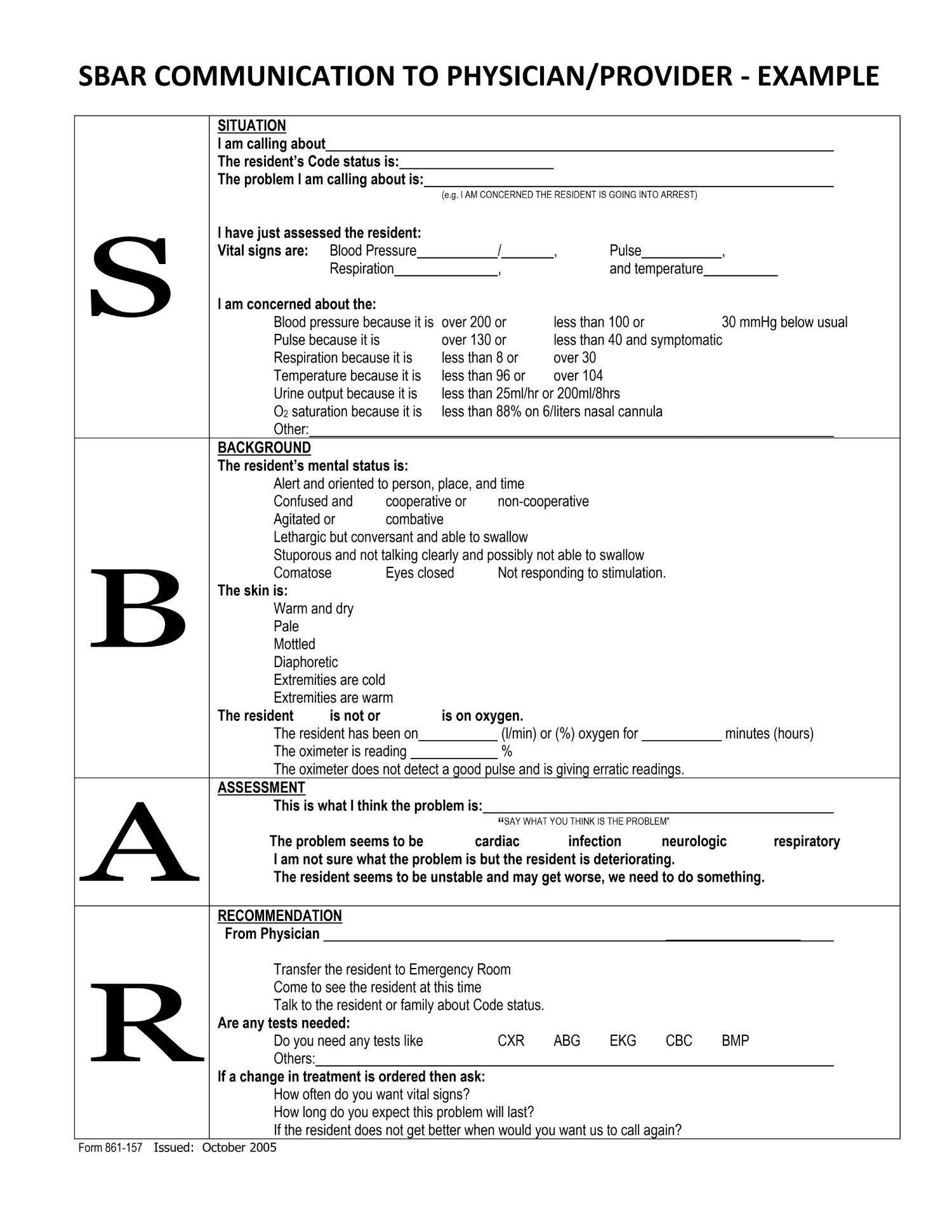
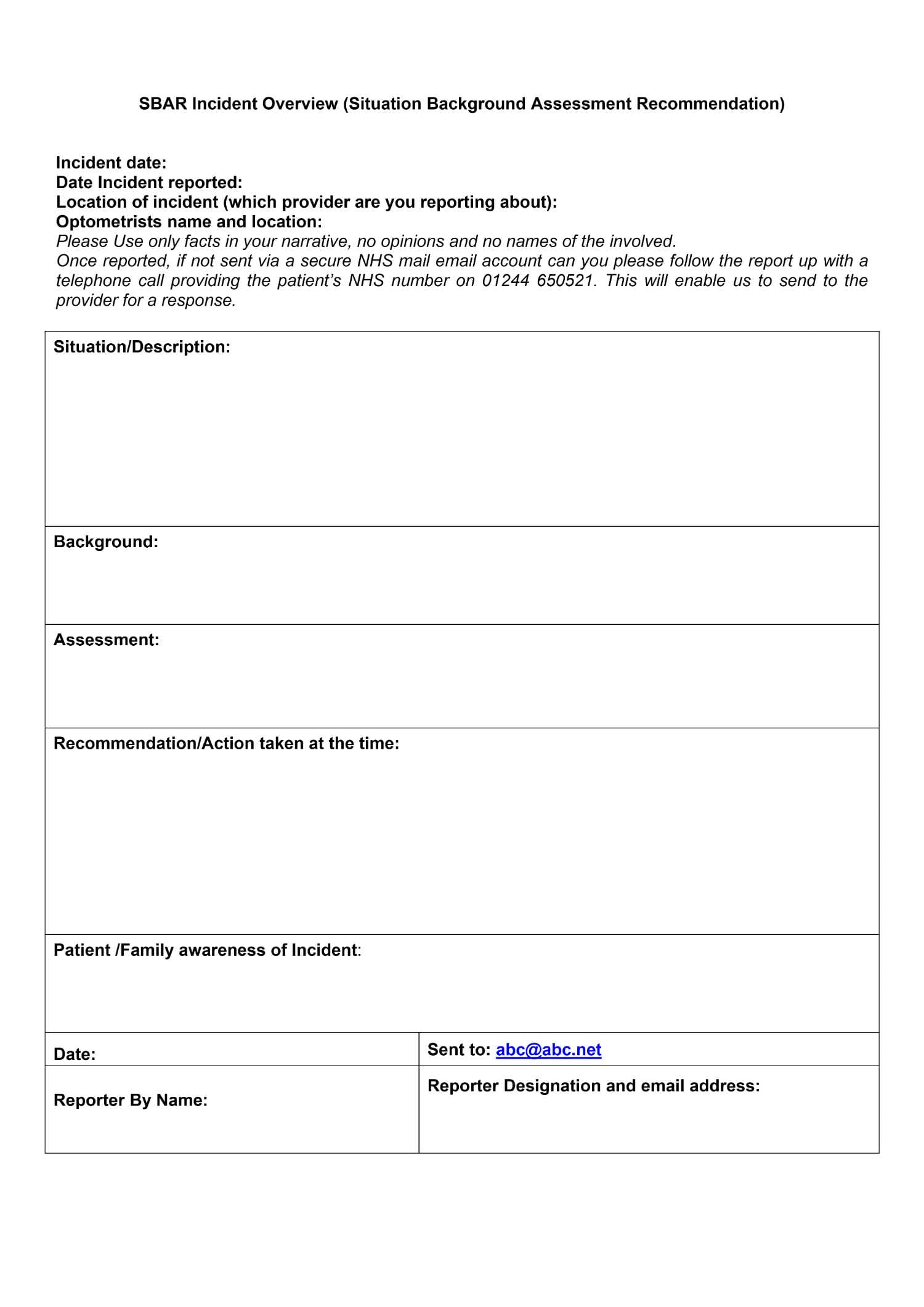
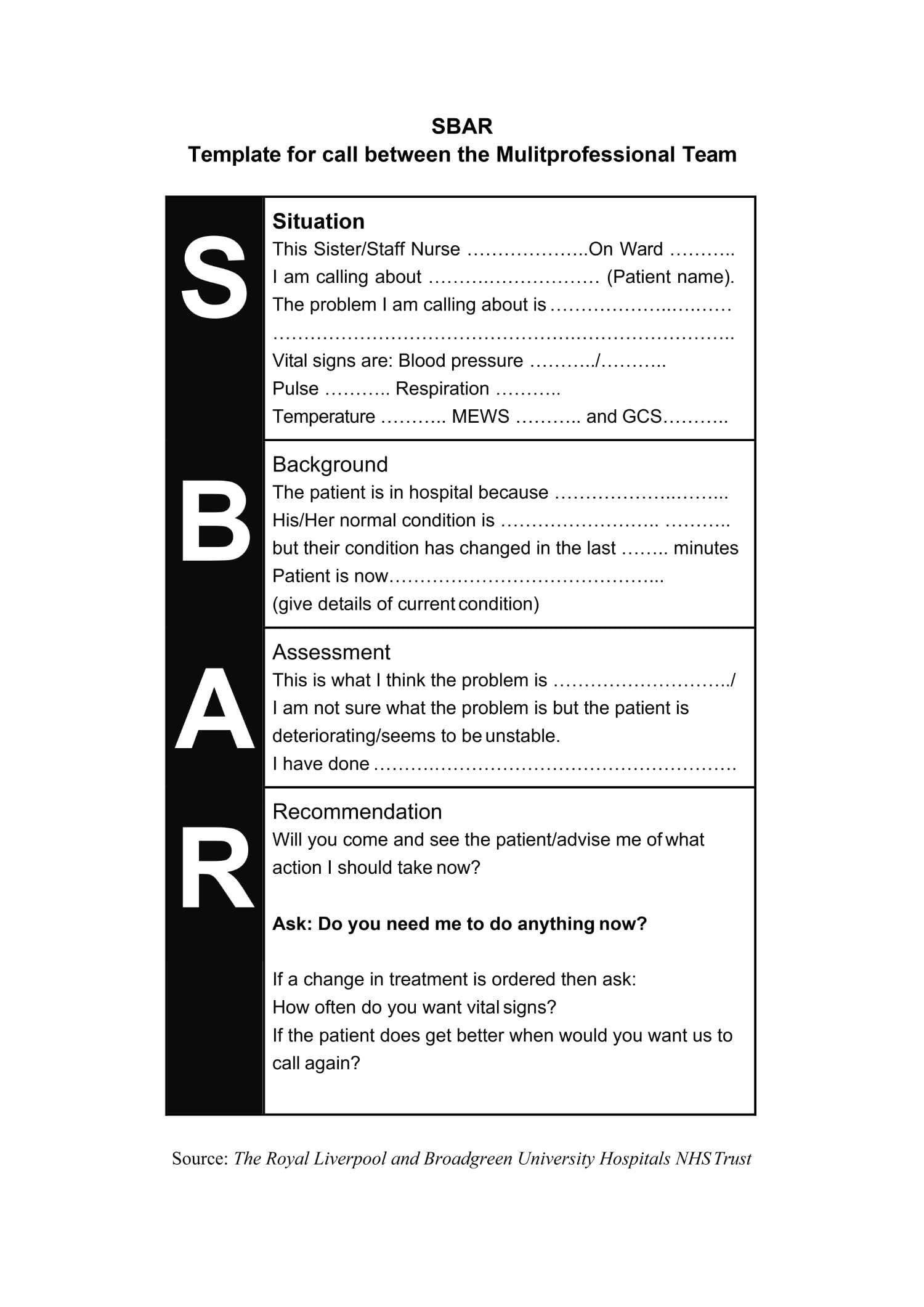
SBAR Template #1
SBAR Template #2
SBAR Template #3
SBAR Template #4
SBAR Template #5
SBAR Template #6
SBAR Template #7
SBAR Template #8
SBAR Template #9
SBAR Template #10
SBAR Template #11
SBAR Template #12
SBAR Template #13
SBAR Template #14
SBAR Template #15
What Is SBAR?
SBAR stands for Situation, Background, Assessment, and Recommendation. It is a fixed sequence that healthcare professionals use to share important patient information. The goal is to make communication brief but complete so the next clinician can understand what is happening and act without delay. SBAR gives every exchange a predictable order, which is especially useful when information must be passed quickly during a busy shift or emergency.
In an SBAR message, the Situation comes first, a short statement describing the immediate concern, such as a sudden change in vital signs or a request for review. The Background adds key clinical details like the patient’s diagnosis, recent procedures, allergies, or medication changes. The Assessment explains the professional’s current impression or concern about the patient’s condition, and the Recommendation states what needs to happen next and how soon, such as ordering labs, adjusting medication, or calling a provider to the bedside.
Clinicians use SBAR in many daily settings such as handoffs between shifts, nurse-to-physician calls, rapid-response activations, bedside updates, and telehealth consultations. It ensures that essential facts are shared in the same order every time, reducing omissions, improving teamwork, and keeping patient information ready for immediate decision-making.
Essential Elements of an SBAR Template
An effective SBAR note is brief, specific, and delivered in the same order each time. The four sections below outline how to describe what is happening now, provide key context, share a concise clinical judgment, and state the action needed with a clear timeframe. Following this sequence keeps every exchange focused and ready for decision-making.
Situation
Start with a short statement explaining why you are reaching out. Identify the patient by name, age, and location, and describe what has changed or prompted concern, including timing and current severity. Highlight only the critical findings that define urgency, such as markedly abnormal vital signs, new chest pain, sudden shortness of breath, rhythm change, or a rapid drop in oxygen saturation. If there is an immediate threat (airway obstruction, active bleeding, altered mental status), say it plainly so the listener recognizes priority right away.
Background
Give brief context that directly relates to the current problem. Mention the admission date and main diagnosis or working concern for today, then add information that shapes interpretation or action: pertinent history, baseline condition, recent procedures, allergies, medications that could influence the event, and key results with timing and values (for example, “Creatinine 2.1 mg/dL today, up from 1.0 last week,” “Chest X-ray this morning shows new right lower-lobe opacity”). Include devices and code status when relevant. Skip details from remote or unrelated history so the message stays practical and focused.
Assessment
Summarize your professional judgment based on current findings and trends. Anchor your statement in observable data such as vital signs, examination findings, output, labs, or imaging, and compare them to baseline where it helps (“worse than yesterday,” “no change after nebulizer,” “fever began at 14:00”). If the diagnosis is uncertain, name your leading concern and the level of concern clearly (“concern for sepsis,” “possible gastrointestinal bleed,” “high risk for deterioration”). Mention any immediate interventions already performed and the patient’s response so the receiver knows what has been done so far.
Recommendation
Be clear about what you need and when. Specify the action, whether a bedside review, diagnostic test, medication change, or transfer, and include the timeframe. Note what monitoring or supportive steps you will continue while awaiting the response (repeat vitals every 15 minutes, maintain continuous oximetry). Confirm how the recipient can reach you and request a read-back for critical items. If appropriate, state what will happen next if no response is received within the expected time window.
How to Use the SBAR Method
In busy clinical settings, SBAR works best when it follows a steady and familiar rhythm. Start by choosing the right channel for communication, such as an in-person conversation, a phone call, or a brief written note, and gather only the facts that guide decisions. Then move through Situation, Background, Assessment, and Recommendation in sequence. The steps below explain how to apply SBAR effectively in daily practice.
Prepare and Decide the Channel
Before you begin, check the patient’s immediate safety and determine urgency. Decide whether to call, speak in person, or create a short written note. Open a blank SBAR or a standard entry in your system, and time-stamp the record.
Pro Tip:
Keep the latest vital signs and monitor readings in view so you can quote exact values with units.
Gather Only What Matters
Collect the few details that influence decisions, admission date, today’s working problem, key history, allergies, high-impact medications, and recent results with dates and units. Add device information (oxygen, lines, drains) and current code status if it applies.
Draft the Situation First
Write one or two sentences that identify the patient and describe the concern. Include timing and current severity.
Example
Stuart Martin, 68, on 3 West. New chest discomfort for 20 minutes with BP 86/54 and oxygen saturation 88% on 2 L.
Pro Tip:
If the request is urgent, include it at the end of this sentence so the listener hears the need early.
Add a Targeted Background
Give the minimum context needed to interpret the situation. Mention baseline status, today’s diagnosis or working problem, recent procedures, allergies, and decisive results with timing and values.
Example
Admitted yesterday for CAP; chest X-ray this morning shows new right lower-lobe opacity; on ceftriaxone and azithromycin; not on anticoagulants; creatinine 2.1 mg/dL today, up from 1.0 last week.
State a Focused Assessment
Share your clinical impression based on current findings and trends. Compare to baseline where useful and note responses to any interventions. If the cause is uncertain, name your leading concern without overstating it, such as “concern for sepsis,” “possible GI bleed,” or “at risk for deterioration.” This communicates reasoning while leaving room for further evaluation.
Make a Clear Recommendation with a Timeframe
Say exactly what is needed and when. Specify the action, bedside review, orders for labs or imaging, medication adjustment, or transfer, and the expected timeframe. Add what you will continue while awaiting a response, such as repeating vitals or continuous pulse oximetry. Include your direct call-back number to speed follow-up.
Deliver the Message and Pause for Confirmation
Speak in short sentences and follow the SBAR order. After giving your recommendation, pause for questions. For critical items or verbal orders, ask for a read-back to confirm accuracy.
Close the Loop
Agree on the next steps, who will carry them out, and when to review. If appropriate, set a backup plan for what to do if the patient worsens or no reply comes by the expected time. Clear endpoints prevent uncertainty during busy shifts.
Document the Exchange
Record your SBAR note with date, time, your name and role, the person contacted, the agreed plan, and any read-back. Use exact numbers and times rather than vague descriptions. This creates a reliable trail and simplifies later handoffs.
Adapt SBAR to the Context
SBAR can be adjusted to match different clinical settings without changing its core order. During a rapid-response call, begin directly with airway, breathing, and circulation before moving through the remaining details. State the urgent request first, such as “immediate bedside review,” so help is mobilized right away. For unit transfers, include the destination, transport needs, current infusions, and any monitoring that must continue in transit. In pediatric cases, list weight and age-specific references since medication doses and vital-sign ranges vary by age. When the update centers on medication, focus on indication, dose, timing, recent changes, and any adverse reactions or monitoring results. In telehealth exchanges, start by confirming the patient’s name, date of birth, and location, and mention any limits to the physical exam so both parties understand what can and cannot be assessed remotely. Adapting details this way keeps communication efficient and appropriate to the situation while preserving the clarity SBAR is meant to provide.
Common Pitfalls to Avoid
Even experienced clinicians can drift from the SBAR pattern under pressure. The most frequent issue is including too much history, which can obscure the main concern. Keep only the facts that influence current decisions and store background notes elsewhere. Another common error is using vague or qualitative language, for example, saying “vitals are low” instead of giving the exact numbers and units. Precision keeps listeners from misinterpreting severity. A third pitfall is delaying the recommendation until the end of a long explanation. In urgent cases, state what you need early so the receiver can act without waiting. Finally, leaving the next step unclear can create hesitation; always close with a named action, a timeframe, and a reliable contact route.
Pro Tip:
Before calling or sending a message, read your SBAR aloud once. If it takes more than about a minute to say, remove details that do not change the plan so the message stays concise and useful.
Is SBAR Evidence-Based?
Yes. SBAR is widely recognized as an evidence-based communication method endorsed by the Joint Commission and supported by numerous studies on patient safety. It was developed to reduce preventable errors caused by incomplete or disorganized communication between healthcare professionals.
Breakdowns in communication remain one of the leading causes of clinical errors. These lapses can arise from outdated technology, unclear reporting habits, or the absence of a consistent format for sharing patient details. SBAR addresses these challenges by giving clinicians a shared way to exchange critical information in the same order every time, whether during handoffs, phone updates, or bedside interactions.
Research has shown that SBAR improves accuracy, reduces repetition, and helps teams respond faster in urgent situations. Nurses and physicians report greater confidence when discussing patient conditions because both parties know what kind of information to expect and in what sequence. For patients who cannot describe their symptoms clearly, SBAR ensures their condition is still communicated accurately, preventing key details from being missed.
By promoting clarity and accountability, SBAR supports a safer environment for both patients and healthcare teams. It turns communication into a coordinated effort where everyone, from bedside staff to consulting specialists, works from the same understanding of the patient’s current state and care needs.
FAQs
Begin by choosing the channel, phone, in person, or a short written note, then gather only details that influence decisions. Start with the Situation in one or two sentences, identify the patient by name, age, and location, describe what has changed, include timing, and note current severity with exact numbers when available. Add a concise Background limited to the current issue, including admission date, working diagnosis, relevant history, key medications, and decisive results with dates and units. Provide a focused Assessment based on today’s findings and trends, and note the response to any steps already taken. End with a clear Recommendation and timeframe, mention what you will continue while waiting, and give a direct call-back number. Deliver the message in short, steady sentences, pause for questions or read-back as needed, and document who was contacted, what was agreed, and when follow-up will occur.
In nursing, SBAR (Situation, Background, Assessment, Recommendation) is a fixed-sequence method for sharing patient information in one concise message. Nurses use it for real-time updates such as handoffs, escalation calls, and brief consults. The order keeps attention on the immediate concern, the context that matters, the nurse’s professional impression, and the action being requested. This consistency prevents omissions, limits back-and-forth clarification, and supports faster agreement on next steps across disciplines. SBAR is intended for short exchanges and complements rather than replaces full documentation in the chart.
List the patient’s name, age, and location, followed by the immediate concern with timing and current severity. Include only details that change decisions, such as markedly abnormal vital signs, rhythm, or oxygen saturation. Add short, relevant context, admission date, working diagnosis, key history, allergies, high-impact medications, and recent results with dates and units. Note devices and code status if applicable. Summarize your clinical judgment based on today’s data and mention any response to interventions already taken. Close with a specific request and timeframe, what you will continue while waiting, and your direct call-back number.
An SBAR report is a short verbal or written summary that presents the Situation, Background, Assessment, and Recommendation in order. It identifies the patient and the main concern, provides just enough background to interpret the change, such as recent history, therapies, or key results with timing and values, and offers a concise clinical judgment. It ends with an explicit request and timeframe, such as a bedside review, new orders, or change in level of care, along with a return contact route. Because it follows a predictable sequence, an SBAR report can typically be delivered in about a minute by phone or fit on a single page when written.
Keep it short, about 30 to 90 seconds when spoken or no longer than one brief page when written. As a guide, aim for four to six sentences in a phone update or 10 to 15 short lines in writing. Use exact numbers, units, and times, and remove background details that do not affect the decision.
SBAR is used any time a quick, reliable exchange about a patient’s status or change in condition is needed. Common examples include nurse-to-nurse handoffs, nurse-to-physician updates, rapid-response activations, transfers between units, consult requests, and telehealth check-ins. It also works well for urgent coordination, new abnormal results, unexpected symptoms, or therapy responses that require prompt review. For ongoing documentation, teams rely on regular chart notes; SBAR is reserved for concise communication that drives immediate action.
No. SOAP (Subjective, Objective, Assessment, Plan) is a documentation style used to record clinical encounters. SBAR is a fast communication sequence for handoffs, escalations, and requests for action. SOAP documents care after it occurs, while SBAR organizes information to prompt an immediate response. Many teams use both, SBAR for the conversation and SOAP for the chart entry.
Final Thoughts
When writing an SBAR, keep your message brief, specific, and ready for decision-making. Start with the immediate concern and current severity, using exact numbers, units, and timestamps. Keep the background limited to facts that guide action, admission date, working problem, key history, major medications, and a few decisive results with dates and values. Add devices or code status only when relevant. Present a focused clinical impression based on today’s findings and note any response to interventions already taken. Close with a clear request and timeframe, what you will continue while waiting, and a direct call-back route. Ask for a read-back when details or orders are critical.
Use the SBAR templates above to make documentation easier and faster. Each template is fully editable in Microsoft Word and Google Docs, so you can revise sections, headings, or examples to match your department’s workflow. Aim for a 30 to 90 second phone report or a short one-page written note, record who was contacted and what was agreed, and apply the same SBAR order across your team to strengthen communication and reduce errors.